Mental health & seniors
Dementia and depression remain as the top two concerns.
With a growing ageing population, there is also concern about seniors and their mental health, including dementia and depression which are said to be the top two mental health concerns amongst seniors.
Ageless Online speaks to Dr Julian Hong, a doctor at DTAP Clinic Group and alternative director of Resilience Collective, who was also a moderator at the 5th Singapore Mental Health Conference in January, about the mental health conditions affecting seniors and how to boost seniors’ well-being:
Can you share more about dementia and depression?
Dementia:
A recent study published overseas in 2018 showed there is a 40-percent increased risk of developing dementia for those seniors who face social isolation and loneliness. Closer to home, there was a recent study led by the Institute of Mental Health (IMH) called the “Well-Being of the Singapore Elderly” (Wise) where 5,000 seniors and their family members were interviewed. It found that one in 10 people aged 60 and above may have dementia.
This rise in dementia is attributed to a rapidly ageing population and also an increased prevalence of cardiovascular diseases such as stroke, obesity, hypertension and diabetes – all of which are risk factors for dementia.
In 2018, about 50,000 people in Singapore have dementia and this number is expected to more than double by 2030.
Depression:
Since 2004, the National University of Singapore’s (NUS) Singapore Longitudinal Ageing Study (SLAS) found that widowed or divorced persons above 65 were more likely to experience depression (22 percent or two in 10), than widowed or divorced persons between the ages of 55 and 65 (13 percent or one in 10). This series of studies also found that seniors living alone were twice as likely as their peers to develop depressive symptoms.
A follow-up report for SLAS in 2012 further demonstrated that one in five elderly persons in Singapore aged 75 and above show signs of depression.
Global figures from the World Health Organization (WHO) say that approximately 15 percent of adults aged 60 and over suffer a mental disorder. Why is that?
There are different risk factors for developing mental health problems at each point in one’s life. Ageing presents fresh sets of challenges to that stage of life and the risk factors for developing mental health problems can be complex.
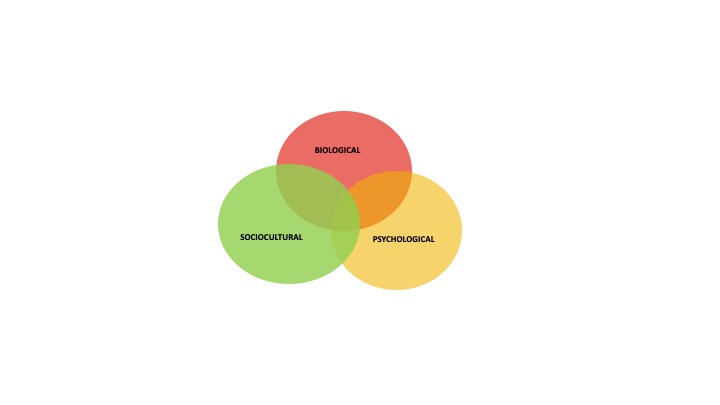
Dr John S Rolland, the co-founder of the Chicago Center for Family Health and an adjunct professor of psychiatry and behavioural sciences at Northwestern Feinberg School of Medicine, US, has a model that explains this well. There are very close interactions between biological, psychological, and socio factors directly related to an individual’s health. Mental health has an impact on physical health and vice versa.
A few examples I have personally come across include:
Biological – My own grandmother had a fall recently and had a fracture. This resulted in her reduced mobility and having to deal with the pain. Having to go through this, affected her mood as she was not able to carry out her daily activities well. Having family support to cheer her up made a huge difference to how she coped with this health concern.
Psychological – Events such as bereavement of a family or friend, or a setback in a hobby or at work – all this can trigger depression. And if seniors have a long-term chronic condition, their ability to care for themselves and their condition can be affected, for instance such as not taking medications or not going for follow-up with their doctors.
I remember one of my patients Mr W who was dealing with a setback at an organisation he ran. The feelings of failure caused him to have a persistent low mood, which resulted in him not being able to enjoy his sex life. This psychological effect resulted in a biological outcome and in turn affected his relationship with his wife (social isolation).
Social – Loss of income through retirement or even loss of work, social isolation as children grow up and leave home, or even the loss of a spouse. Humans are social beings and thrive in relationships.
Central to this social need as well is a healthy sex life, even as one ages. Hormonal changes experienced through ageing can impact this and a change in sex life does affect one’s relationship with his or her spouse, in turn causing emotional and psychological distress as well.
Looking after seniors goes beyond the confines of the clinic. Personally, I believe in empowering them to age with dignity and most importantly, a family-first approach in addressing their biological, psychological and social needs.
But what happens when family is not in the equation? What advice would you give?
It is honestly more challenging when families and immediate loved ones are not in the picture. Whilst some are lucky to have close friends, others may often face social isolation. The last line of defence is thus the social safety net, depending on befrienders (such as non-profit Lions Befrienders), Pioneer Generation ambassadors, and grassroots to identify these socially-vulnerable elders and connect them to meaningful groups in the community so they can receive support and not fall through the cracks. If you know someone socially-isolated without family in their lives whether it is their choice or not, your reaching out to them can make a huge difference in their life.
Do you feel some of the figures above could be more as it is mostly under-reported as some are reluctant to seek help?
A lot of the previous numbers I quoted are from studies which started in the early 2000s. And the prediction of an increase in an elderly population and their concomitant health struggles will lead to a greater number of seniors facing mental health challenges.
NUS Medicine’s Community-based Early Psychiatric Intervention Strategy in 2008 found that only 12 percent (one in 10) of seniors who had depressive symptoms sought professional help, while 75 percent (three in four) did not see themselves as having a mental disorder.
The awareness of mental health challenges amongst seniors isn’t well discussed nor often addressed. This lack of insight and awareness results in family members and seniors not recognising the signs and symptoms, and also not knowing how to get help. So yes, the figures could likely be under-reported.
What advice can you give to those who may have mental health problems?
If you are caregiver of a senior or a senior yourself, it is important to look out for these warning signs and symptoms:
For depression:
- Persistent feelings of sadness for more than two weeks.
- Loss of interest in things you used to enjoy.
For dementia:
- Memory loss that starts to affect one’s daily life, such as not remembering the way home.
If you suspect yourself or the person you are caring for having these early warning signs, it will be useful to speak to a doctor to get further assessment. There are medications to take to bring depression to a state of remission (cure), however for dementia, there is no cure except to slow down the progress of the disease.
What are some ways to boost seniors’ mental health and well-being?
Active ageing is important, in fact it is a national thrust by our Government on ageing gracefully. I share some advice on the same bio, psycho and social perspectives that we discussed earlier:
Biological:
- Regular health checks – If you are above 60 and have not had a health screening before, it is useful to see your doctor to explore having one done. Picking up any chronic diseases early can ensure early treatment and control, preventing any further consequences.
- Manage chronic diseases – If you have a chronic disease like high blood pressure, cholesterol or diabetes, please also ensure you are on regular follow-up and taking your medications regularly.
Psychological:
- Awareness of depression or dementia – Mood and memory are an important part of our daily life. If you find yourself having a persisting low mood, not enjoying the things you use to usually enjoy for more than two weeks, or if you find yourself developing memory loss that is interfering with your daily life, please speak to your doctor for further assessment.
- Strengthening family ties – I discussed earlier on the importance of a family-first approach as family forms the first line of support, especially for a senior. Starting small, one can celebrate important occasions with your family such as birthdays, important events, etc. Or simply by being there for your family when they need you.
- Spousal intimacy – A big factor in ageing is the hormonal changes one experiences. These hormonal changes can affect sexual function, libido and resultantly spousal intimacy. Speaking to a doctor who has experience in men’s or women’s health can help address these hormonal changes as you age.
Social:
- Meaningful work, lifelong learning and volunteering in the community – One of the big risks predisposing one to dementia or depression in seniors is social isolation and continuing to enjoy one’s work and contributing give seniors a sense of purpose and dignity; lifelong learning keeps the mind active such as learning a new hobby or skill; and volunteering allows one to give back his or her time and experience, and make a difference.
As we discussed earlier, each of the bio, psycho and social aspects are interlinked and affect each other and all three of these components need to be looked after and addressed concurrently. Most importantly, seniors need to know that they are not walking this journey alone and they have a raft of support from their families, their healthcare providers and even their employers as we move towards an ageing-friendly Singapore.



Prevention is far better than cure. As we age, plaques appear between brain cells thus causing communication breakdown between brain cells. As more brain cells communication breakdown, the result is dementia. So, to prevent dementia is to remove these brain plaques from forming by taking daily 2 teaspoonfuls of coconut oil into a bowl of rice at meal time or one spoonful of tumeric powder into a bowl of soup. This has been proven to be very effective in USA. As an analogy, how far can one drive a car without any maintenance at all ?